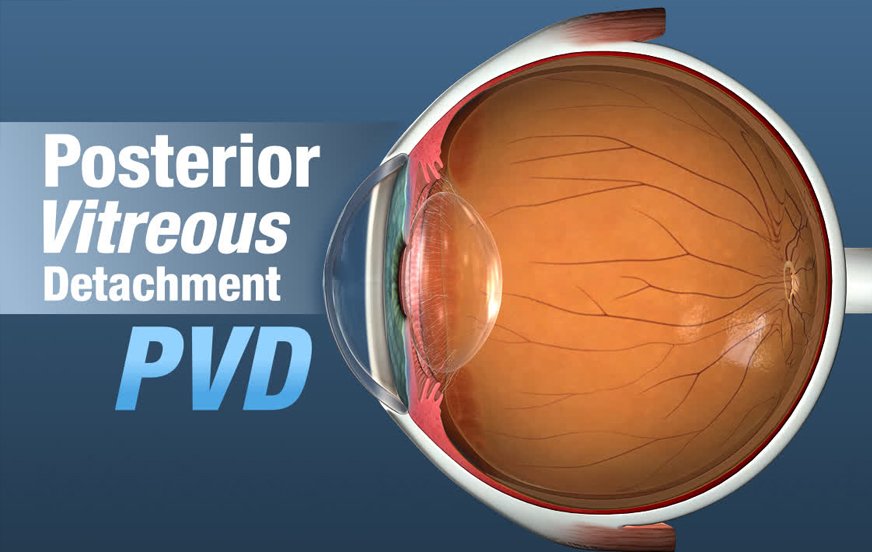
Posterior vitreous detachment- (PVD) Bharti eye foundation
The translucent fluid that makes up your eye’s vitreous detachment is present throughout. The vitreous maintains the form of your eye. This is not a concern because we can still see pretty well without the vitreous connected to the retina. When the vitreous gets too soft, it loses its shape, turns away from the retina, and contracts inward toward the center of the eye. PVD happens frequently and naturally. You won’t lose your vision; most of the time, no treatment is necessary.
The symptoms of PVD?
Despite the possibility of additional symptoms, PVD does not result in pain or irreversible vision loss. They include are:
- Flashes. These brief bursts of light resemble the “stars” you experience after hitting your head. When detachment is complete, they typically come to an end or stop happening altogether. They may be short or long.
- Floaters. These moving things in your field of vision may look like tiny particles, dust, spots, or dark, cobweb-like items. During the first few weeks of PVD, the best approach to finding them is to look at a light surface, such as the sky or a white wall.
- Cobweb effect. As the vitreous separates from the retina, you could start to notice its outside. You can feel like you’re searching through cobwebs. This only lasts until detachment is complete, at which point it vanishes.
Causes of PVD?
The main factor for PVD is aging. The vitreous has a harder time keeping on its original shape as you age. The vitreous gel decreases and becomes more liquid-like in consistency, but the distance between your lens and retina remains the same.
Most people get PVD after the age of 60, while it can occur younger. Less likely to occur in those under the age of 40.
Typically, PVD affects both eyes. If you have a vitreous left eye, you could also develop a detachment in your right eye.
Risk factors for early PVD include:
- cataracts
- eye surgeries
- diabetes
- An eye injury.
- nearsightedness
How to diagnose PVD
Despite the reality that PVD is common, it’s crucial to visit a doctor if you have any new floaters or flashes. A retinal detachment or PVD may be the cause of these. To diagnose your problem, your doctor might need to perform a diagnostic test.
PVD, a retinal detachment, or another eye condition may be confirmed by a dilated eye exam. Your ophthalmologist or optometrist will put special drops into your eyes during the examination. Your doctor can view the back of your eyes due to these drops since they make your pupils bigger. The entire retina, the macula, and your optic nerve can then be examined by your doctor.
About 30 minutes pass during the examination. The dilatation can last for a few hours until it goes away. After your appointment, you should put on a pair of sunglasses because the sun and bright lights could be uncomfortable.
What is the treatment for PVD?
Usually, PVD doesn’t need to be treated.
Usually, it takes no more than three months to fully detach. After the detachment process is over, if you still experience floaters, talk to your doctor about your treatment options.
If any of the following symptoms start to appear, you could require additional treatment:
- Continued floaters. You could require a vitrectomy if you frequently see floaters or have vision problems. Some or all of the vitreous gel inside the eye is removed during this outpatient treatment.
- Retinal tears. If the fibers of the vitreous pull on the retina too strongly, the underlying tissue may tear in one or more spots. Retinal detachment may happen if fluid gets underneath the retina. If unattended, it may result in eyesight loss. Both a retinal tear and a retinal detachment can be treated surgically.
- Macular spots. These occur when the retina is tightly attached to the vitreous as it pulls away. They result in foggy, distorted eyesight. Macular holes that don’t sometimes close on their own, but surgery can close them.
How can I reduce my floaters?
If you have a visible floater, gently rotating your eyes may be helpful. This can sometimes relocate the floater out of your line of vision, making it less visible while the vitreous inside your eyes is being moved.
If your optometrist has recommended glasses, wearing them as needed will make it easier for you to see what you’re doing. You’re more likely to be able to focus on the task at hand rather than on the floaters when your vision is sharper.
In bright light, sunglasses will help you see your floaters less clearly. Your floaters will leave a paler shadow on your retina since the tinted lenses let less light into your eyes.
Reduce the brightness of the screen to see if your floaters become less annoying when you’re using a computer or tablet.
What activities I am still able to undertake despite having PVD?
The majority of people with PVDs are unrestricted in their ability to engage in daily activities. High-impact exercise is advised to be avoided for the first six weeks after the onset of a PVD, according to some ophthalmologists. This is due to the possibility that your vitreous has not fully separated from your retina, and you may be more susceptible to developing a retinal detachment at this time.
Although there is no proof that any of the following activities will unquestionably lead to PVD issues, some persons may be advised to avoid them or choose to do so:
- Extremely strenuous or high-impact exercises like jogging or aerobics.
- Playing contact sports, such as rugby, martial arts, or boxing.
- Inverted postures are used in exercises like yoga or pilates.
Always consult with your ophthalmologist regarding which activities and for how long you should refrain from engaging in them. The advice you receive may depend on whether your retina is thought to be particularly in danger.
If you do engage in any of these activities, you might become much more aware of your floaters. This is due to the fact that these activities need you to move about, which can cause your floaters to move around inside your eye more. As a result, you might want to put a stop to such activities until your brain adjusts and learns to disregard your floaters.
You can continue doing things like walking, light exercise, reading, watching TV, cooking, and using your computer on a daily basis. There is no evidence to support the idea that taking an aircraft can aggravate or worsen your PVD. Additionally, wearing makeup or contact lenses has no impact on your PVD.
Do PVDs have any complications?
In the majority of PVD patients, the vitreous separates from the retina gently, without any issues, and does not affect your vision permanently. Only a very small percentage of patients may have difficulties as a result of their PVD.
Conclusion
Age-related PVD is a common eye disease that typically doesn’t require treatment.
Don’t self-diagnose if you start to develop eye or vision issues. It’s critical to see an eye doctor for a diagnosis and treatment because the symptoms of PVD might resemble those of other dangerous eye conditions.
Make sure to arrange a yearly appointment for a routine eye exam. Regular check-ups enable the early detection and treatment of eye or vision issues.
READ MORE:
This article is posted here





